On July 7, 2022 the Centers for Medicare and Medicaid Services (CMS) officially released the 2023 Quality Payment Program (QPP) proposed rule. The 2,066 page proposed rule contained many changes that may take place in the 2023 MIPS performance year and beyond.
This blog post breaks down the proposed changes to the QPP and MIPS for 2023.
Performance Thresholds
CMS is proposing to maintain the threshold to avoid a penalty at 75 points for 2023.
As required by the Bipartisan Budget Act of 2018, the 2022 performance year/2024 payment year is the last year for the exceptional performance bonus. Beginning with the 2023 performance year, there will not be an exceptional performance threshold or bonus.
Proposed thresholds:
- Threshold to Avoid a Penalty: 75 points
- Exceptional Performance Threshold: Retired (as required by law, 2022 was the last year)
CMS is proposing no changes to the threshold to avoid a penalty and the exceptional performance bonus has been retired.
Category Weights
CMS is not proposing changes to performance category weights in 2023.
Quality Category
CMS is proposing the following beginning in 2023:
- Measure Scoring
- For large practices (>15 clinicians), remove the 3-point floor for measures meeting data completeness and case minimum. These measures would be scored on a 1-10 point scale instead of a 3-10 point scale.
- For small practices, the 3-point floor will remain.
- Bonuses
- No change to the small practice bonus or the improvement score bonus.
- Measures: For pertinent measure changes, review our Top 2023 Proposed MIPS Changes Report.
CMS is proposing the following for the 2024-2025 performance years:
- Data Completeness Threshold
- Increasing from 70% to 75%.
Cost Category
No significant changes proposed.
Improvement Activities
No significant changes proposed for scoring or reporting this category. There are, however, several proposed changes to the list of improvement activities (IAs), including:
- Four proposed new IAs, including Create and Implement a Language Access Plan (high-weighted) and COVID-19 Vaccination for Practice Staff (medium-weighted).
- Five changes proposed to existing IAs, including Use of QCDR data for ongoing practice assessment and improvements.
- Five proposed removals, including use of QCDR for feedback reports that incorporate population health (high-weighted).
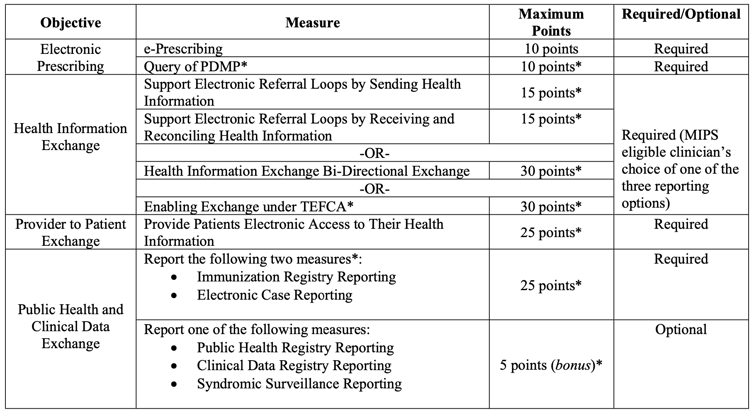
Promoting Interoperability (PI)
In 2020, CMS finalized that clinicians can only use certified electronic health record technology (CEHRT) that meets certification requirements. On December 31, 2022, in order to remain certified, an EHR must meet the conditions of the Cures edition update. Because of this, you must be using an EHR certified to the 2015 Edition Cures Update for your 90-day PI performance period in 2023.
CMS is proposing the following beginning in 2023:
- New Required Measure: Query of Prescription Drug Monitoring Program
- This was previously an optional bonus measure.
- This measure is being expanded to include Schedule II opioids and Schedule III or IV prescriptions (previously only Schedule II).
- There are 2 proposed exclusions:
- You are unable to electronically prescribe Schedule II opioids and Schedule III and IV drugs under applicable law during the performance period.
- You write fewer than 100 permissible prescriptions (Schedule II opioids and Schedule III and IV drugs) during the 90-day performance period.
- Change to the Public Health and Clinical Data Registry Objective
- Proposals would require you to report which stage of engagement you are in with the registries ("Pre-production and Validation" or "Validated Data Production")
- In order to get credit for being in active engagement with the required or bonus registries, you would only be allowed to be in Pre-production and Validation for a maximum of 1 year, after which you would need to progress to Validated Data Production.
- The exception is if you switch between 1 or more registries. Those new registries that you switched to would be allowed to be in Pre-production and Validation for 1 year. attest to both the Immunization Registry Reporting measure and the Electronic Case Reporting measure to get credit. (Unless an exclusion applies).
- For the required Electronic Case Reporting measure, exclusion 4 (your CEHRT that is not certified to the electronic case reporting certification criterion at § 170.315(f)(5) prior to the start of the performance period they select in CY 2022) will not be available beginning in 2023.
- New Option to Satisfy the Health Information Exchange Objective
- In addition to currently available options (Sending and Receiving measures or the Bilateral Exchange measure), CMS proposes to add a third option: Participation in the Trusted Exchange Framework and Common Agreement (TEFCA).
- TEFCA is new this year and very few avenues of participation exist. If finalized, it is unlikely that many clinicians will be able to use this option in 2023.
- In addition to currently available options (Sending and Receiving measures or the Bilateral Exchange measure), CMS proposes to add a third option: Participation in the Trusted Exchange Framework and Common Agreement (TEFCA).
- New Category Scoring to Accommodate New Measure
MIPS Value Pathways (MVPs)
MVPs will roll out in 2023 for the first time. There are no MVPs currently relevant to our specialists.
Next Steps
- Register for our July 20 webinar on the 2022 MIPS proposed changes.
- Review our Top 2023 Proposed MIPS Changes Report for a quick rundown of major MIPS changes relevant to our specialties.
- Subscribe to our newsletter to get alerts on this and other important issues. You can subscribe using the field in our website footer below.
- If you are not a MarsdenAdvisors client, contact us to learn more about our MIPS Success Plan and to reap the rewards of our combined decades of experience.
If you want hands-on, personalized assistance, contact us and we will have your back.

