On July 23, 2021 the Centers for Medicare and Medicaid Services (CMS) officially released the 2022 Quality Payment Program (QPP) proposed rule. The 1,740 page proposed rule contained many changes that may take place in the 2022 MIPS performance year and beyond.
This blog post breaks down the proposed changes to the QPP and MIPS for 2022.
Performance Thresholds
CMS is proposing to increase both the threshold to avoid a penalty and the exceptional performance threshold in 2022. These increases reflect statutory requirements that, beginning with the 2022 performance year, the threshold to avoid a penalty must be equal to the mean or median score from a prior year and that the exceptional performance threshold must be set to the 25th percentile of final MIPS scores from the prior year that are above the 2022 performance threshold.
Proposed thresholds:
- Threshold to Avoid a Penalty: 75 points
- Exceptional Performance Threshold: 89 points
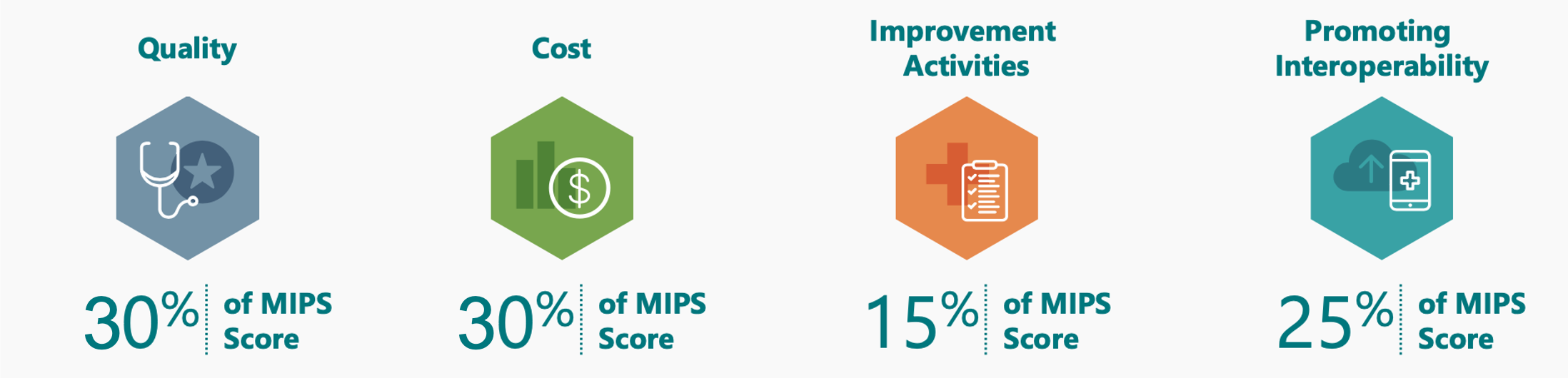
Category Weights
CMS is proposing to set both the Quality and Cost category weights to 30% in 2022. This change is required by law and so will be finalized as proposed.
Quality Category
CMS is proposing the following beginning in 2022:
- Measure Scoring
- For large practices (>15 clinicians)
- Measures that have a benchmark, meet case minimum, and meet data completeness will be scored on a 1-10-point scale instead of a 3-10-point scale.
- Measures not meeting the above criteria will earn 0 points.
- For small practices
- Measures that have a benchmark, meet case minimum, and meet data completeness will be scored on a 1-10-point scale instead of a 3-10-point scale.
- Measures not meeting the above criteria will earn 3 points.
- For large practices (>15 clinicians)
- Benchmarks: Given the profound impact of COVID-19 in 2020, CMS is concerned that they will not reliably be able to use 2020 performance rates to calculate 2022 benchmarks. Quality measure benchmarks are usually calculated using the performance rates from the performance year 2 years prior.
- For performance year 2022, CMS proposes to either use benchmarks based on 2019 performance (the same benchmarks used in MIPS this year) or to calculate benchmarks based on 2022 performance data.
- Bonuses
- Remove the outcome/high priority measure and end-to-end electronic reporting bonuses.
- No change to the small practice bonus or the improvement score bonus.
- Measures: For pertinent measure changes, review our Top 2022 Proposed MIPS Changes Report.
Beginning in 2023, CMS proposes to increase the data completeness threshold to 80%.
Cost Category
CMS is proposing five new episode-based cost measures for 2022 MIPS. The list includes one measure on Melanoma Resection (10 episode case minimum) and one on Diabetes (20 episode case minimum). These two measures could impact our dermatology and ophthalmology clients. If you received one, we recommend reviewing your August 2020 field test report for these measures.
Improvement Activities
No significant changes proposed for this category.
Promoting Interoperability
CMS is proposing the following beginning in 2022:
- Small Practice Hardship: Small practices would automatically have the PI category reweighted (no application required). If the practice reports PI data, the category will be scored.
- New Required Measure: SAFER Guides
- Much like the Security Risk Analysis, this measure, though required, would not be scored.
- Attestation would require annual SAFER High Priority Practices self-assessment.
- Change to the Provide Patients Electronic Access to Their Health Information Measure
- Would require you to ensure that patient health information remains available to the patient (or patient-authorized representative) to access indefinitely and using any application of their choice that is configured to meet the technical specifications of the API in your EHR.
- This would apply to all electronic patient data from date of service January 1, 2016 onward.
- Change to the Public Health and Clinical Data Registry Objective
- Would require you to attest to both the Immunization Registry Reporting measure and the Electronic Case Reporting measure to get credit. (Unless an exclusion applies)
- If you claim an exclusion for both required measures, this objective's 10 points would be redistributed to the Provide Patients Electronic Access to Their Health Information measure.
- If you report on either both required measures or if you report on one required measure and claim an exclusion for the second:
- You would receive 10 points for the objective
- You would be able to report one additional measure from this objective (including registry-EHR integration) to receive 5 bonus points for the PI category.
- Would require you to attest to both the Immunization Registry Reporting measure and the Electronic Case Reporting measure to get credit. (Unless an exclusion applies)
MIPS Value Pathways (MVPs)
The rollout of MVPs will be delayed until 2023.
Next Steps
- Register for our August 19 webinar on the 2022 MIPS proposed changes.
- Review our Top 2022 Proposed MIPS Changes Report for a quick rundown of major MIPS changes relevant to our specialties.
If you want hands-on, personalized assistance, contact us and we will have your back.

