On November 2, 2021 the Centers for Medicare and Medicaid Services (CMS) released the 2022 Quality Payment Program (QPP) final rule. The 2,414 page final rule contains many changes that will take place in the 2022 MIPS performance year and beyond.
This blog post provides our instant analysis of the high-level finalized changes to the QPP and MIPS for 2022. In the coming weeks, we will provide more comprehensive analyses of the rule and what it means for you.
Performance Thresholds
CMS is finalizing an increase to both the threshold to avoid a penalty and the exceptional performance threshold in 2022. These increases reflect statutory requirements that, beginning with the 2022 performance year, the threshold to avoid a penalty must be equal to the mean or median score from a prior year and that the exceptional performance threshold must be set to the 25th percentile of final MIPS scores from the prior year that are above the 2022 performance threshold.
Finalized thresholds:
- Threshold to Avoid a Penalty: 75 points
- Exceptional Performance Threshold: 89 points
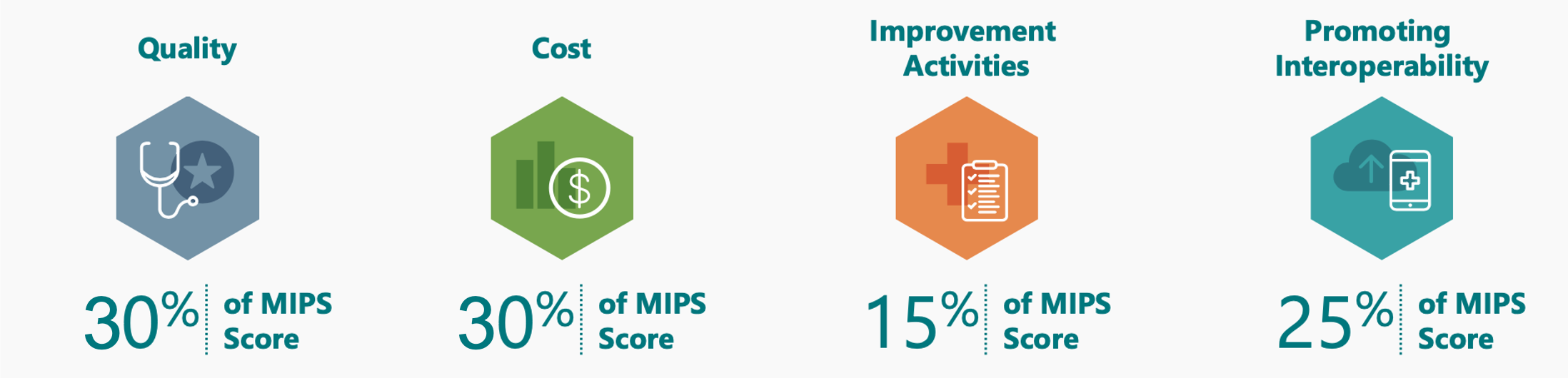
Category Weights
CMS has finalized a change to set both the Quality and Cost category weights to 30% in 2022. This change was required by law.
Quality Category
CMS has finalized the following beginning in 2022:
- Measure Scoring
- For new measures, there will be a 7-point floor for their first year in MIPS and a 5-point floor for their second year in MIPS.
- Benchmarks: No change from previous policy.
- For performance year 2022, CMS will use historical benchmarks using 2020 performance period data.
- Bonuses
- Remove the outcome/high priority measure and end-to-end electronic reporting bonuses.
- No change to the small practice bonus or the improvement score bonus.
- Measures: For pertinent measure changes, review our Top 2022 Final MIPS Changes Report.
CMS has finalized the following beginning in 2023:
- Measure Scoring
- For large practices (>15 clinicians)
- Measures that have a benchmark, meet case minimum, and meet data completeness will be scored on a 1-10-point scale instead of a 3-10-point scale.
- Measures not meeting the above criteria will earn 0 points.
- For small practices
- Measures that have a benchmark, meet case minimum, and meet data completeness will be scored on a 1-10-point scale instead of a 3-10-point scale.
- Measures not meeting the above criteria will earn 3 points.
- For large practices (>15 clinicians)
- Data Completeness Threshold
- No change: will remain at 70%. CMS had proposed, beginning in 2023, increasing the data completeness threshold to 80%.
Cost Category
CMS finalized the addition of five new episode-based cost measures for 2022 MIPS. The list includes one measure on Melanoma Resection (10 episode case minimum) and one on Diabetes (20 episode case minimum). These two measures could impact our dermatology and ophthalmology clients. If you received one, we recommend reviewing your August 2020 field test report for these measures.
Improvement Activities
No significant changes finalized for this category.
Promoting Interoperability
CMS has finalized the following beginning in 2022:
- Automatic Small Practice Hardship: Small practices would automatically have the PI category reweighted (no application required). If the practice reports PI data, the category will be scored.
- New Required Measure: SAFER Guides
- Much like the Security Risk Analysis, this measure, though required, would not be scored.
- Attestation would require annual SAFER High Priority Practices self-assessment.
- No Change to the Provide Patients Electronic Access to Their Health Information Measure
- In response to our feedback, CMS chose not to finalize the proposed new requirement that you ensure that patient health information remains available to the patient (or patient-authorized representative) to access indefinitely and using any application of their choice that is configured to meet the technical specifications of the API in your EHR.
- Change to the Public Health and Clinical Data Registry Objective
- Requires you to attest to both the Immunization Registry Reporting measure and the Electronic Case Reporting measure to get credit. (Unless an exclusion applies)
- If you claim an exclusion for both required measures, this objective's 10 points will be redistributed to the Provide Patients Electronic Access to Their Health Information measure.
- Requires you to attest to both the Immunization Registry Reporting measure and the Electronic Case Reporting measure to get credit. (Unless an exclusion applies)
-
- If you report on either both required measures or if you report on one required measure and claim an exclusion for the second:
- You will receive 10 points for the objective
- You will be able to report one additional measure from this objective (including registry-EHR integration) to receive 5 bonus points for the PI category.
- If you report on either both required measures or if you report on one required measure and claim an exclusion for the second:
MIPS Value Pathways (MVPs)
The rollout of MVPs will be delayed until 2023.
Next Steps
- Keep an eye out for an announcement of our 2022 QPP and MIPS Final Rule webinar in the coming weeks.
- Review our Top 2022 Final MIPS Changes Report for a quick rundown of major MIPS changes relevant to our specialties.
If you want hands-on, personalized assistance, contact us and we will have your back.

