For those that submitted Merit-Based Incentive Payment System (MIPS) data for 2021, you are now able to view your performance feedback and final score through the Centers for Medicare & Medicaid Services (CMS) Quality Payment Program (QPP) website.
Let's review what the performance feedback consists of, how to access your performance feedback and final score, as well as what to do if there is an issue with your final score.
Performance Feedback
Performance feedback is a summary of data CMS has collected from your submission and includes measure-specific information, as well as information about payment adjustments. You can expect your performance feedback to include:
- Measure-level specific data and scores
- Activity-level scores
- Patient-level measure reports (if applicable)
- Performance category-level scores and weights
- Final score
- Payment adjustment information
- Payment adjustments will be applied to Medicare Part B covered services Paid amounts.
- Payment adjustments will not be applied to:
- Non-assigned claims for services.
- Covered professional services furnished during the payment year by a new Medicare-enrolled eligible clinician.
- Medicare Part B drugs or other items and services that aren't covered professional services.
For some MIPS participants, there is a new section of the performance feedback called "Patient Risk Factor Data". This section is for informational purposes, and will include information about your patients' medical complexity and social risk in comparison to other MIPS eligible clinicians. This information is partly what CMS uses to create your complex patient bonus score. As of now, this section is not available for APM entities.
How to Access Your 2021 MIPS Final Score and Performance Feedback
If you already have an account, you'll need to have your login credentials handy.
-
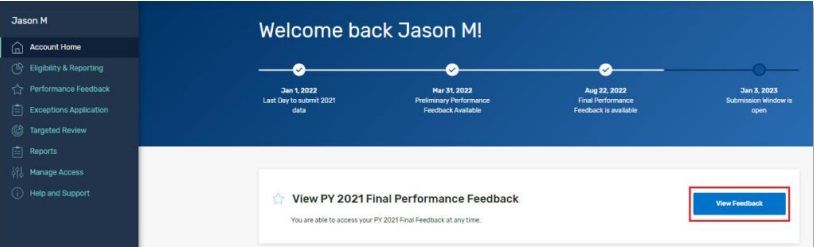
Log in to your Quality Payment Program account.
-
Once signed in, click on "View Feedback" button to the right.
-
If there is an issue with clicking the button highlighted above, you can also click the "Performance Feedback" section on the left-hand navigation.
If you are a new user, you'll need to go to QPP account registration page and complete the form to create an account. Registration should take five to 15 minutes, according to CMS. You can watch this handy video guide on how to create a QPP account and review our guide on how to connect your account to your organization.
Notice an Error?
If you believe there is an error with your score, you can request a targeted review up until October 21, 2022 at 8 pm ET.
Some examples of targeted review relevant circumstances are:
- Data was submitted under the wrong Taxpayer Identification Number (TIN) or National Provider Identifier (NPI)
- Eligibility or special status issues (e.g., you have Qualifying APM Participant status and shouldn’t receive a payment adjustment)
- Performance categories weren’t automatically reweighted even though you qualify for reweighting due to extreme and uncontrollable circumstances
If you are a MarsdenAdvisors client:
We are reviewing our clients' 2021 MIPS final scores and 2023 payment adjustments and will reach out with details.
If you aren't a MarsdenAdvisors client:
- Contact us for information on how to benefit from our combined decades of experience, OR
- You can go through the targeted review process yourself
- CMS recommends contacting their QPP service center before submitting a targeted review request, as some errors can be addressed outside of the targeted review process, or could be applicable to more entities than just you.
- You can contact the QPP Service Center at 1-866-288-8292 (Monday-Friday, 8 a.m. - 8 p.m. ET) or by e-mail.
- If the error is not resolved, you can submit a targeted review by October 21, 2022 at 8 pm ET using the instructions in the 2021 Targeted Review Guide.
- CMS recommends contacting their QPP service center before submitting a targeted review request, as some errors can be addressed outside of the targeted review process, or could be applicable to more entities than just you.
Next Steps
- Share this information with your practice colleagues.
- Subscribe to our newsletter to get alerts on this and other important issues. You can subscribe using the field in our website footer below.
- Contact your Client Success Manager if you have any questions.
- If you’re not a MarsdenAdvisors client and you want hands-on, personalized assistance, contact us and we will have your back.
If you have any questions on this, let us know!

